Pelvic Organ Prolapse - Female
If you are reading this then you are probably being proactive to prevent or improve prolapse.
"Pelvic organ prolapse (POP) refers to loss of support for your organs leading to an altered position of one or more of your organs into your vagina." (Source page 57)
Your support comes from your pelvic floor muscles, ligaments and a web of tissues.
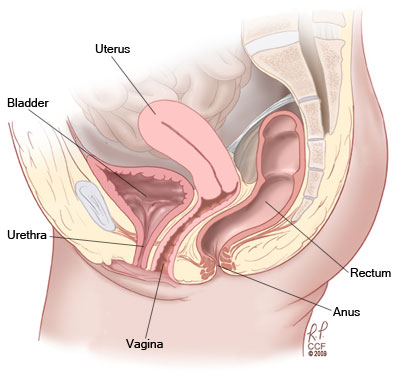
Your organs are your bladder, urethra, uterus, vagina, bowel and rectum.
Wear and tear on your supporting tissues can lead to prolapse.
You may experience one of more of the following:
- the feeling of a lump (“something coming down”),
- low backache,
- heaviness,
- dragging sensation,
- or the need to push on or near the prolapse in order to empty your bladder or bowel.
The position and your awareness of your prolapse can change from morning to evening and day to day depending on your activity level.
You will often notice it more at the end of the day, after long periods of standing, lifting, carrying or exercise and less when you are lying.
Prolapse may be more prominent at times of abdominal straining e.g. coughing or straining to empty your bowels.
The picture below shows a stage 2 bladder prolapse. This is also known as an anterior vaginal wall pelvic organ prolapse.

The picture below shows a back vaginal wall prolapse.
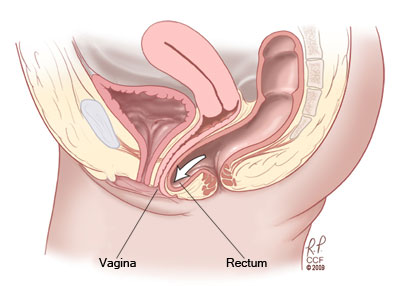
Other types not shown here are womb (uterus) and top of your vagina prolapse after hysterectomy.
What causes or worsens prolapse?
Prolapse is caused or worsened by:
- Pregnancy and childbirth. More vaginal births, more risk.
- Straining to empty your bowels.
- Hysterectomy increases the risk of prolapse.
- Vaginal hysterectomy and hysterectomy performed for pelvic organ prolapse are the strongest risk factors for having more pelvic floor surgery.
- Strenuous exercise, heavy lifting.
- Smoking and chronic cough.
- Being overweight
- Chronic Anaemia
- Vitamin D deficiency
- Thoracic kyphosis
- Hypermobility also known as being double jointed.
- Ageing process
How common is prolapse?
Based on women reporting a feeling of a mass bulging into the vagina, pelvic organ prolapse has about a rate of 5 and 10 out of every 100 women. (Source page 57)
There is an estimated lifetime risk of surgery for prolapse of 7% to 11%. (Source page 59)
Will it get worse?
A study of 161,000 post menopausal women suggests that prolapse is not always long standing and progressive.
Spontaneous improvement is common, especially for stage 1 prolapse.
Progression was less common in women of normal weight.
Progression was more common in women who had more pregnancies and births. (Handa et al 2004)
So what do I do?
Below is a government link that summarises treatment options for pelvic organ prolapse.
Australian Commission on Safety and Quality in Health Care - POP consumer information sheet
Your physiotherapist can help you understand, implement and maintain the lifestyle changes and pelvic floor exercises mentioned here.
These take time to work and need to be continued over your whole life.
Assessment
Assessment at Innerstrength is very holistic so be prepared to answer a variety of questions about your bladder, bowel, pelvic floor and sexual situation.
Diagnosis is usually done using examination to identify which part of your vagina has moved.
Your physiotherapist will be able to give you an idea of the stage of your prolapse, when you are lying.
If you haven't already had an examination please read the Informed Consent For Examination - Female form before arriving at your next appointment and be ready with questions.
If you feel comfortable your physiotherapist can assess your proplapse whilst you squat or stand to get a more accurate idea of what you are expereincing.
Dealing with the diagnosis
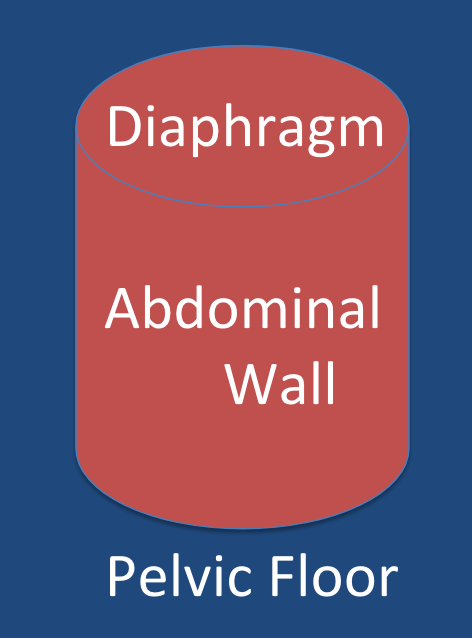
What is Intra-abdominal pressure?
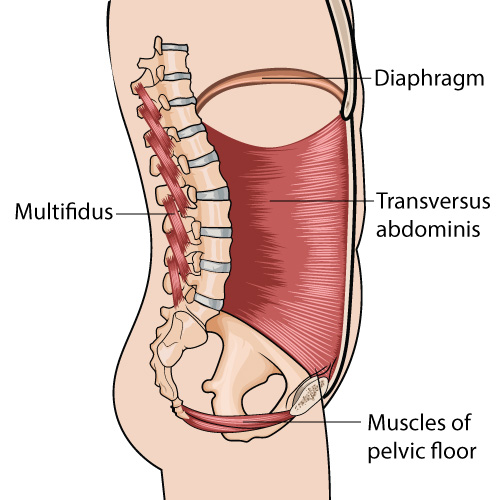
Pelvic floor and Prolapse

The boat is uplifted and supported by the water and the moorings are loose.
Similarly your organs are uplifted by your pelvic floor & your tissues are loose.
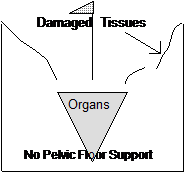
If there was no water, the boat would sink and the moorings strain and break.
This is most likely to happen slowly and progressively and be felt more after straining to open bowels, heavy lifting, at the end of the day, after exercise or when you have cough or sneeze alot.
What is my pelvic floor?
How can I manage or prevent prolapse?
These strategies will prevent further prolapse while you improve the active support of your organs.
If you choose to have surgery these suggestions will help you prepare and recover from surgery.
Do
Pelvic Floor Muscle training - Your physiotherapist will take you through your Intensive Personalised Pelvic Floor Rehabilitation Programme.
Empty your bladder completely.
Rest - Intermittent lying down or lying with your bottom in the air if your are bothered by the dragging sensation.
Low impact exercise - consider lower impact choices such as cycling, swimming or walking.
Use prescribed vaginal oestrogen
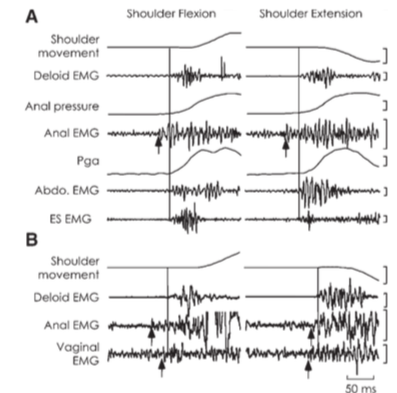
Learn Dynamic pelvic floor Bracing(The Knack)- your physiotherapist will teach you how to lift your pelvic floor muscles dynamically as you move to lift your organs and protect your tissues.
Don't
Strain to empty your bowel or bladder.
Lift heavy objects especially from the floor (see below)
Stand for prolonged periods if this worsens your dragging feeling
If your bladder or bowel emptying has been affected by your prolapse your physiotherapist will help you manage this.
Sometimes improving your bladder and bowel emptying takes months to years to achieve.
Also you can read and discuss how to empty your bladder with your physiotherapist at your next appointment.
Also you can read and discuss normal bowel habits with your physiotherapist at your next appointment.
Lifting (toddlers or other objects)
Can I continue to have sexual intercourse with a prolapse?
Yes if it is comfortable. Be very generous with your use of personal lubricants.
Click here to read more abou Personal Lubricants.
How effective are pelvic floor exercises for prolapse?
Please click here to read about the level of evidence for the role of pelvic floor exercises in improving or managing prolapse.
How do I do pelvic floor exercises?
What exercise can I do?
What happens if I cannot do pelvic floor exercises?
What happens if lifestyle changes and pelvic floor muscle exercises don't work?
If this is you then you have the following choices.
- Live with it.
- Try a pessary
- Try Surgery
Do I have to have surgery?
-
Lifestyle changes
-
Pelvic floor exercises
-
Pessary
-
Surgery
What is a pessary?
Tell me more about Surgery
Financial Assistance
Click here for information about financial asistance
Your questionnaires to track your progress
Pelvic Organ Prolapse Symptom Score
Pelvic Floor Muscle Exercise - Self Efficacy
Transvaginal Mesh complications support services
In Victoria, a Mesh Information and Help Line is available by calling 1800 55 6374 (1800 55MESH).
The information line is supported by the Continence Foundation. Calls are returned for all messages left, within 24 hours.
Safer Care Victoria has published information and provides links to important information such as credentialing and freedom of information resources on the public website:
www.betterhealth.vic.gov.au/health/ConditionsAndTreatments/Transvaginal-mesh
Specialist multidisciplinary services are provided at:
Royal Women’s Hospital Phone: 03 8345 3143
Mercy Hospital for Women Phone: 03 8458 4500
Monash Health Phone: 03 9928 8588
Western Health Phone: 0481 908 118
Services at these hospitals include:
- Mercy Hospital for Women. A multi-disciplinary team provides services for affected women. Services include urogynaecology, urology, colorectal surgery, pain management and community linkage with psychiatric services.
- Monash Health. The Pelvic Floor Unit leads care, in conjunction with physiotherapy, pain management, and where indicated, colorectal, urology and plastic surgery. Other specialised services include psychology, a sexual and relationship difficulty clinic, and a continence nursing service.
- Royal Women's Hospital. Urogynaecology is the lead discipline, with services such as plastic surgery, urology and colorectal surgery are also involved, depending on patient needs. Patients can also access pain physicians and physiotherapists.
- Western Health. Services include urogynaecology, urology, colorectal surgery, pain management and community linkage with psychiatric services. The lead discipline is urogynaecology with a multidisciplinary clinic involving urology, pelvic floor physiotherapy and continence nursing.
