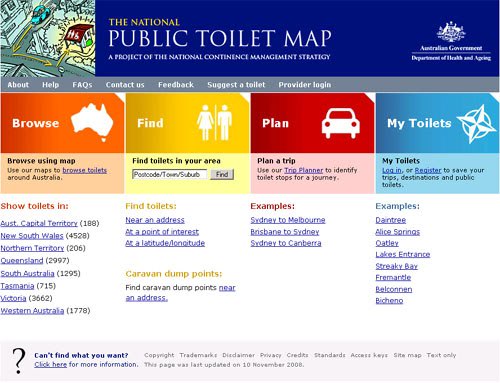
Click here to visit the Toilet Map Website where you can find a nearby toilet or plan your next journey.
The terms for common bladder problems can be confusing.
They are decided upon by international committees to reduce confusion and improve research.
Sometimes it takes a while for the rest of the world to catch up and health professionals use old terms.
Complaints or symptoms are descriptions of your experience.
A diagnosis is a combination of complaints and medical tests.
Complaints
Urgency (urinary) incontinence is the complaint of involuntary loss of urine associated with urgency.
Urgency is the complaint of a sudden, compelling desire to void which is difficult to defer.
Overactive bladder (OAB) syndrome is urinary urgency, usually accompanied by frequency and nocturia, with or without urgency urinary incontinence, in the absence of urinary tract infection or other obvious pathology.
Diagnosis
Detrusor Overactivity
Detrusor Overactivity is a diagnosis (by symptoms and urodynamic investigations) made in women with lower urinary tract symptoms.
It is when involuntary detrusor (bladder) muscle contractions occur during filling cystometry.
These contractions, which may be spontaneous or provoked, are unable to be suppressed by the patient.
Bladder Oversensitivity
Bladder oversensitivity, a diagnosis made by symptoms and urodynamic investigations, is more likely to occur in a women with symptoms of frequency and nocturia, and a voiding diary showing a clearly reduced average voided volume.
Women typically complain of an early first desire to empty, an early strong desire to void, which occurs at low bladder volume, no bladder spasm and no UTI.
The following problems are assocated with urinary urgency.
Childhood incontinence and bed wetting
Straining to empty your bladder or bowel
Not relaxing your pelvic floor to empty your bladder
Habitually stopping and starting when emptying your bladder
Not waiting to finish emptying your bladder
A history of ignoring bladder sensations
A history of holding your pelvic floor tightly
Hovering in a squat position over the toilet seat
Excessive caffeine consumption
Anxiety, Stress, Sexual, Physical and Emotional abuse.
A loaded full bowel
A history of Urinary Tract Infections
Excessive abdominal effort when trying to hold on.
Back pain
Most people with bladder problems understand that when their daily stress increases so too do their bladder complaints.
Evidence and understanding of the role of stress in bladder problems is growing.
In one study urinary frequency, urgency, and nocturia were associated with previously experienced sexual, physical, and emotional abuse for both genders and for all ethnic groups.
In another study, 31% of women with OAB reported almost twice as often earlier physical or sexual abuse as did the women with stress urinary incontinence (18%) or women without urinary symptoms (18%.)
In an Iranian study, individuals with OAB had more anxiety and depression as did another multinational study where increased depression and anxiety scores were found among individuals with OAB
Furthermore, postpartum depression has also been reported to be associated with urgency incontinence.
This is a stressful problem and is associated with anxiety, trauma and stress.
This is such a vicious circle.
A vaginal and perineal examination is a really important part of your initial assessment.
Please fill in your questionnaire before every appointment.
Your bladder and bowel affect each other in three ways.
- They are in very close together and a full bowel can affect your bladder.
- Your nervous system controls both your bladder and bowel.
- Your bladder and bowel share ligaments and tissues that hold them in place.
Straining to empty your bladder and bowel negatively affects and stretches tissue and nerves.
Tell your physiotherapist if you have irregular bowel motions or trouble emptying.
You may need to alter your
fluid amount and type it is best to do this in discussion with your physiotherapist after completeing your bladder diary.
It is important that you empty your bladder completely.
Refer to How to empty your bladder
female or male and use the techniques listed there.
If you are having trouble emptying your bladder to completion then you may be asked to double void
female or
male
Practice Diaphragmatic Breathing so you are able to use it to control your urge anywhere, anytime.
Pelvic floor control
Pelvic floor muscle control and
rehabilitation is the basis of bladder retraining.
For some the goal is to learn to contract your pelvic floor and others the goal is to learn to relax.
Click here for more information about your pelvic floor:
Men,
Women Practice your personalised pelvic floor muscle exercises so you are able to use them to control your urge anywhere, anytime.
Did anyone ever tell you it was mind over matter and just "Hold on"
Whilst for some people this may be helpful, this advice may make you worse.
It really depends on how much you drink and the average size of each empty.
It is very important to do a bladder diary and change your behaviour based on fact.
Did anyone tell you “Don’t sit on public toilet seats”?
They used to think it would save you from infections.
Now we know the opposite is true.
Hovering above the toilet seat may increase the chance of urinary tract or bladder infections.
This is because your bladder doesn’t empty.
Carry a small pack of wet wipes to wipe the seat, if you are concerned, and sit.
Did anyone tell you “Go just in case”?
This was to save your parents from having to find a public toilet.
You and your sibling’s bladders were little and you went often and unpredictably.
Now you are older you know where the toilets are located.
Ask your physiotherapist if you should go without an urge.
Did anyone tell you “Stop start your flow.”
The practise of stopping and starting your urine flow used to be taught as a way to do pelvic floor muscle exercises.
This is no longer recommended as it was found that this results in incomplete bladder emptying and may increase the likelihood of Urinary Tract Infections (UTIs).
Bladder retraining should be done with supervision of your physiotherapist and only after you have completed your
bladder diaryBladder retraining helps you change your bladder behaviour.
With courage, perstistance and determination you can achieve permanent change.
Persistence is needed as it takes time and there will be “ups and downs.”
There are a variety of ways to retrain your bladder
- You may be asked to do timed toileting where you empty your bladder at regular intervals before urges.
- You may learn to suppress the urge and then go to the toilet immediately.
- You may learn to suppress the urge and defer or hold on.
- Later you may start to tackle the triggers such as running water, cold, and getting home and putting the key in the door.
A strong urge usually comes over you like a wave.
Many people who experience these overwhelming body sensations and leakage understandably go into "fight flight" or panic.
Unfortunately the body response of "fight flight" can result in you bending, inhaling and drawing in your abdominal muscles.
This response can do the exact opposite of what you need to do.
Imagine the action of getting sauce out of a sauce bottle.
This "fight flight" response can result in a downward pressure on your bladder.
This is not helpful.
With courage, perstistance and determination you can learn to ride this wave until it settles.
Try the following.
Stay still and remain calm.
Relax your belly/abdomen
Learn, practise and use
diaphragm breathing.
Lift your pelvic floor and keep breathing
Then proceed calmly to the toilet.
Try this at home first to build confidence and then start to use it in more situations.
For some it helps to avoid those strong urges all together for a short time.
Your physiotherapist will tell you if this is a good stategy for you.
Timed voiding involves toileting at fixed schedule intervals.
For example:
Start with emptying your bladder every hour during waking hours.
Continue this for a week.
When you feel confident you have some control over the urge, have less leakage episodes and can follow the schedule with minimal interruptions you may be ready to progess.
To progress expand the time between bladder empties by 10 to 15 minutes per week.
Continue increasing the time between bladder empties each week until a two to three hour voiding interval is achieved.
A shorter or longer initial toileting interval may be necessary depending on the result of your bladder diary.
For example:
One hour may be way too long to wait and so 30 minutes is your starting point.
Deferring is only necessary if your bladder chart showed that you have a small bladder capacity and you are emptying fully.
This is generally not the first way to tackle your bladder problem.
You will learn to choose which urge is a genuine full bladder urge and which is a bladder tickle/spasm.
You could decide to delay going until the urge is stronger or returns.
Hypnosis and Psychology are now recognised treatments in the management of stress and trauma.
The type of therapies are hypnosis, mindfullness meditation, aceptance committment theories and cognitive behavioural therapies.
Jo Sheedy Psychologist at Innerstrength Physiotherapy is happy to help.
Diaphragmatic Breathing has an audio track that you can use to interupt some of the stressful thoughts and interupt your focus on your bladder.
If you bladder can be triggered by running water, putting the key in the door, arriving at the toilet or cold weather, you are not alone.
This is not fully understood but we do know these are learned associations.
Associations means that your brain links one experience with another.
Associations were first described in the famous experiment called Pavlov's dog.
Pavlov's dog initially was repeatedly exposed to the ringing of a bell before being offered food.
Pavlov's dog quickly learned to associate the bell with food.
He was found to salivate when he heard the bell.
Humans make associations as well.
This is a survival skill and it is just learning.
We certainly remember when something we experience results in strong emotions of shame and embarassment.
Urgency or incontinence make us feel threatened as they are socially taboo.
We make associations and learn quickly.
If you leaked once getting home, you may have made an association.
Getting home then may trigger a bladder contraction and the urge to empty your bladder.
It is possible to break down the association through repeated small less threatening exposures.
If running water triggers an urge.
Here is a desensitisation program that you can practice 2-3 times/day.
Progress to the next step if you have no urge or a mild urge.
Immediately after emptying your bladder, run the tap and feel the water and give yourself positive feedback for not getting an urge.
If you are getting a strong urge use your diaphragmatic breathing, relaxed belly, pelvic floor contractions, or the TENS machine to suppress the urge.
-
Next run the tap 15 minutes after emptying your bladder and give yourself positive feedback for not getting an urge.
- Extend the time out gradually increasing the gap by 15 minutes every 2-3 days.
- In a few weeks you should be able to stand by a running tap 2 hours after emptying.
- The next stage is to wait 2 hours after emptying your bladder, this time drink some water and then turn on a tap.
- Lastly repeat step 4 but drink whilst the tap is running.
Don't worry if you have a relapse, just go back a few steps and stay on that step for a week and progress more slowly.
If getting home triggers an urge.
Use your urge suppression techniques.
Try a different entrance.
Go to the toilet before your leave to travel home.
You could also try to distract yourself when you get in the door and do one small activity such as putting your key or bag away before going to the toilet.
You could do a number of these small activities before going to the toilet.
You could then challenge yourself by gradually increasing the time between your last empty and arriving home.
If you are getting a strong urge use your diaphragmatic breathing, relaxed belly, pelvic floor contractions, or the TENS machine to suppress the urge.
Don't worry if you have a relapse, just go back a few steps and stay on that step for a week and progress more slowly.
If urgency increases en-route to the toilet
Many people experience leakage as they walk into the toilet.
This can be especially tricky as you get up in the morning.
Try the following to dissociate the toilet from urgency
- Go back to the toilet 20-30 minutes after emptying your bladder and sit as if you are about to urinate but DON'T.
- Extend the time after emptying your bladder by 15 minutes every 2-3 days and continue to sit as if you are about to urinate but DON'T.
If you are getting a strong urge use your diaphragmatic breathing, relaxed belly, pelvic floor contractions, or the TENS machine to suppress the urge. Don't worry if you have a relapse, just go back a few steps and stay on that step for a week and progress more slowly.
Click here for some information about financial assistance for your bladder problem.
For evidence for the various treatments see here.